 Dr. Bruce Perry, MD (left) documents the brain science of how attachment problems can cause developmental trauma to a fetus, infant, or child – just when the brain is developing.
Dr. Bruce Perry, MD (left) documents the brain science of how attachment problems can cause developmental trauma to a fetus, infant, or child – just when the brain is developing.
And he’s taking his “attachment first” approach to Washington. In “Trauma Impacts the Brain: Healing Happens in Relationships,” Perry leads a full-day Pre-conference University on Sunday May 4, to kick off the National Council for Behavioral Health’s Annual Conference ’14 on May 5-7 (click here for details).
“Experiences profoundly influence the development of young children. Adverse Childhood Experiences (ACEs) shape the brain’s organization, which, in turn, influences the emotional, social, cognitive, and physiological activities,” the conference website notes.
“So often, trauma happens in relationships, but it is also in relationships that healing occurs. Explore the latest research and clinical treatment with trauma researcher, treatment visionary, and bestselling author of The Boy Who Was Raised as a Dog, and Born for Love: Why Empathy is Essential and Endangered, Dr. Bruce Perry.”
Dr. Perry’s relationship and attachment theory healing model first assesses each child as an individual, using his Neurosequential Model of Therapeutics (NMT). He emphasizes that there is no one label for child trauma. Rather, “there are very individualized patterns of exposure to trauma (all with unique timing, nature, and patterns)… So we don’t call ‘it’ anything,” he wrote me recently. “We describe it — and try to ‘illustrate’ each individual’s trajectory separately” with the NMT’s individualized brain mapping technique. [FN1]
Dr. Perry recommends his books above as the best summaries of his work. His latest research and key slides are online from his National Council webinar last fall, “Helping Children Recover from Trauma,” National Council LIVE, Sept. 5, 2013 (scroll down to Sept. 2013.) I really recommend this – and it will only be online through August 2014.
Click here for an overview video: [FN2]
Survival Brain Develops First
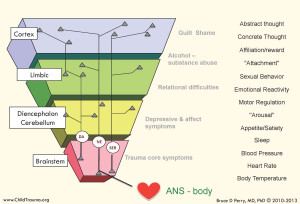 Dr. Perry says we’ve got to learn about the neuro-biological growth of the brain in order of time sequence from conception to later development in infancy and childhood.
Dr. Perry says we’ve got to learn about the neuro-biological growth of the brain in order of time sequence from conception to later development in infancy and childhood.
His “Four Part Brain” slide (above) shows the time sequence from the bottom up: first the brain stem develops (pink); then the diencephalon cerebellum (yellow); they make up our primitive reptilian “survival” brain. Next develop the emotional limbic brain which only mammals have (green), and finally the thinking brain aka frontal cortex (blue).
The fetus’ “survival brain” develop first, because infants require breathing, heart beat, and other survival functions at birth, Dr. Perry told a March 2013 UCLA conference. The rest of the brain develops largely after birth and as an outgrowth of the brain stem. [FN3]
So injury during brain stem development in the first 45 months harms development of the entire brain, the neurons around the viscera, and most of the body.
Dr. Perry next details three key threats to an infant’s developing brain: Trauma in utero (intra-uterine insult); post-birth attachment trauma; and other post-natal trauma – all before the thinking brain comes on line around age 3.
A fetus in utero is designed to develop in nurturing oxcytocin and other “reward” chemicals released by a mother supported by her family, all joyous a baby is coming. Intra-uterine insult occurs when the mother instead uses substances, or is under stress so that her stress hormones impact the fetus’ developing brain. This can be visible stress to the mother: domestic abuse, work stress, violence.
A fetus, however, can also be subject to stress chemicals with no visible external stress to the mother, as in mothers who are anxious, themselves victims of attachment disorder, don’t want a baby, etc. Often these mothers have no steady pattern to their heart rate, and since a baby’s brain grows according to the mother’s heart rate rhythm, the baby’s brain develops dysregulated.
All these “causes a cascade of mental and physical problems in every part of the body and brain,” Perry says. “Every part of the whole brain these neurons enervate will be dysregulated.”
Birth: the Mother of All Stress
Attachment trauma occurs easily because birth is incredibly stressful to a baby: suddenly there’s lack of oxygen, blinding light, shocking cold, terrifying noise, and pain. This floods a baby with stress hormones — which is essential because now it’s not having needs met as in the womb; thus it’s got to protest so someone comes. “If animals in the wild didn’t feel the stress of hunger they’d just lie around and die of starvation,” Perry notes.
 If all goes as designed, an attuned mother meets the baby’s needs, feeds it, swaddles it, turns down the lights, so the baby feels safe and is flooded with reward optiates like oxytocin. If animals didn’t feel opiate rewards when they get up and eat just what they need (not dirt, for example), they’d not get up.
If all goes as designed, an attuned mother meets the baby’s needs, feeds it, swaddles it, turns down the lights, so the baby feels safe and is flooded with reward optiates like oxytocin. If animals didn’t feel opiate rewards when they get up and eat just what they need (not dirt, for example), they’d not get up.
Then they wouldn’t survive, so the stress hormones and the reward opiates are linked. “At the relief of hungry-thirsty-cold stress, we feel pleasure,” Dr. Perry says. An attuned mother “has a well-organized neurobiology to create a healthy organized neural network for the infant of attachment and regulation…
“And in the arms of that caregiver, that is that magic moment literally weaving together the neurobiology of all these different systems. The biology of attachment is that a baby learns by thousands of good experiences that this stress is tolerable because it leads to reward, and this pleasurable outcome is cathexsized to a person, Mom… Ultimately just seeing or hearing Mom makes you feel safe and pleasurable. Let a wounded soldier talk to his mom, he’ll need 45% less pain meds.”
Or not.
If mom instead is under too much stress herself to meet needs, has too many children and no support, or herself was raised by a mis-attuned mom, “she doesn’t get reward from responding to her baby’s distress,” Perry continues. “So the pull to respond isn’t there.”
Even if no stress to the mother is visible, “if she merely meets physical needs, without involving her own pleasure systems, then the weaving together of meeting needs and the reward/safety system is weak or absent. So her baby learns that stress can be life-threatening, that stress is terrifying,” Dr. Perry concludes. [FN3 op. cit.]
The “Or Not” baby’s brain learns: “that’s all she wrote.”
It develops in a state of perpetual stress in which the stress chemicals simply do not stop and the reward chemicals never or seldom come. In this state, fight/flight cortisol flood eventually leads to “freeze” dissociation, Judith Herman reported back in 1992. [FN4]
More Perry slides at: http://attachmentdisorderhealing.com/how-your-brain-works-101/
———————————
Medical Disclaimer: This website is for general information purposes only. It is simply my own research. Individuals should always see their health care provider or licensed psychotherapist before doing anything which they believe to be suggested or indicated herein. Any application of the material on this website is at the reader’s discretion and is the reader’s sole responsibility.
Comments are encouraged with the usual exceptions; rants, political speeches, off-color language, etc. are unlikely to post. Starting 8-22-16, software will limit comments to 1030 characters (2 long paragraphs) a while, until we get new software to take longer comments again.
Footnotes
FN1 Perry, B.D. and Hambrick, E. (2008), “The Neurosequential Model of Therapeutics (NMT),” in Reclaiming Children and Youth, 17 (3) 38-43; and
Dobson, C. & Perry, B.D. (2010), “The role of healthy relational interactions in buffering the impact of childhood trauma in “Working with Children to Heal Interpersonal Trauma: The Power of Play,” (E. Gil, Ed.) The Guilford Press, New York, pp. 26-43
Both at: http://childtrauma.org/nmt-model/references/
FN2 Bruce Perry MD, Daniel Siegel MD, et.al, “Trauma, Brain & Relationship: Helping Children Heal,” www.youtube.com/watch?v=jYyEEMlMMb0 – introductory video on Attachment Disorder and development trauma. Copies at www.postinstitute.com/dvds.
FN3 Perry, Bruce D., MD, “Born for Love: The Effects of Empathy on the Developing Brain,” Annual Interpersonal Neurobiology Conference “How People Change: Relationship & Neuroplasticity in Psychotherapy,” UCLA, Los Angeles, March 8, 2013 (unpublished).
Library of articles on interventions, trauma, brain development: https://childtrauma.org/cta-library/
Training in NMT Method and Somatosensory Regulation, Power of Rhythm — Individual and Site Training Certification Programs, DVD/streaming training, and online training: http://www.ctaproducts.org
Dr. Perry’s latest research and key slides: “Helping Children Recover from Trauma,” National Council LIVE, National Council on Behavioral Health, Sept. 5, 2013 at www.thenationalcouncil.org/events-and-training/webinars/webinar-archive/ (scroll down to Sept. 2013.)
Dr. Perry’s YouTube channel with educational videos in depth: https://www.youtube.com/channel/UCf4ZUgIXyxRcUNLuhimA5mA?feature=watch
FN4 Herman, Judith, “Trauma and Recovery,” Basic Books, New York, 1992
![]()

There are many ways to deal with a cerebrum cortex brain. Some people find that it helps to visualize things in a more clear way, others find that it helps them focus better, and still others find that it can be calming and helpful. It really depends on what works best for you. https://www.healthmassive.com/cerebrum-cortex-brain/
Pingback: Connection -The Key To Healing From Trauma - MindKind Mom
Pingback: #26- Childhood Trauma, Spirituality, and Collaboration with Chris Wojdak, LPC, MT-BC – Creative Therapy Umbrella
My mothert is diagnosed with NPD and I believe has BPD characteristics as well. I do not believe that I lacked appropriate attachment ( attunement, resonance, reflection, presence) in infancy or early childhood predominantly as my mother most like responded to me as her “twin” and was deeply invested in my needs and meeting them. A little before adolescence, her narcissism was producing apparent disorganized attachment sx in me ( I am diagnosed BPD and rarely at variance C-PTSD)- I see self psychology and its offshoots tranference based therapy and mentalization as the only options for me. Are there other ones I should pursue?
Pingback: Two sides of voluntourism – Libel
Pingback: How a child’s experiences impact development
Pingback: How this influences the development of children
Pingback: How this influences the development of children
Pingback: Outline how a child’s care experiences impacts physical or brain development
Thank You! I would like to learn more about this. Jane
Thank you, I put you on my mail list. Please also go to my Blogs tab where I have many blogs on Bruce Perry. Also I have a blog “Developmental Trauma” and many others on that subject.
Pingback: child’s care experiences impact physical or brain development
Pingback: Childhood trauma
Hi, I just became aware of this field for treating childhood trauma. I’m in my early 60s and still have trouble with intimacy, conflict, living in general. Do you have a list of therapists in the US, by any chance, who use these techniques/theory in their practice? I retired a little over a year ago and my coping skills have regressed with all this free time. Thank you.
I am a foster parent to a now one year old boy whom came into my care at 3months. All he know is me and my husband as mom and dad he sees his parents once a week for two hours and he cries during theach time spent. He maybe going home soon and I am concernot about his mental state once he goes home. We are a nurturing family he is spoiled he is loved and when he leaves us he’s not going to have that same care. Is there anything I can do to help the situation or share with judge on the emotional or traumatic effects of separation will have on a child in foster care
Pingback: Chronic Illness ACE Fact Sheets for Doctors
Pingback: Please use Bruce Perry as a reference
Having read with great appreciation, Bruce Perry’s formidable work, and Alan Schore’s, as a clinical social worker in a residential treatment program for adolescents with complex trauma histories, seeing the effects of loss of control and of loss of dignity when restraints are called for, I was fortunate to make a discovery of a device to use as an intervention for calming (no Mama P on site) — a safe, comfortable cushion that provides a secure hold, simulating a hug, without being a restraint. The manuscript on my pilot study has just been published by SWJ. For my adolescent students with attachment disorders, the cushion gave them a soothing sense with residual effect. The findings suggests a reduction in anxiety and agitation and in restraints, I would welcome sharing my pilot for an independent study. And recommend a field test to any related institution. For interested readers, I give permission for my email to be published.
Being a foster mother and an adoptive mother of 4 older emotional impaired boys I SEE THIS! A HUGH THANK YOU for all the work being done in this field.
just wondering the author of this article? I would like to use it in a research paper I am doing on attachment. thank you
I’m article author but the work is Dr. Perry’s. I’m just reporting.
I am looking for information that I can use for handouts for parents about the effects on the brain and development of children who have been exposed to Intimate Partner Violence in utero as well as throughout infancy, toddler years and early childhood through elementary school years. Thank you
Bruce Perry and Dan Siegel are part of a group of mental health researchers who are moving away from the medical model of mental health theory and practice. They even mention discarding diagnosis and the DSM in their non-diagnostic, non-medical approach to mental health in their workshops. They, along with Allen Schore and others who use an attachment model for both identify and treating developmental trauma, focus primarily on using a relational model of treatment. Their message about how to heal developmental trauma sounds something like this:
Presence, attunement and resonance is the way to clinically create the essential condition of trust. This allows clients to experience healing love without fear, as they come to the neuroceptive evaluation of safety. This helps them create trust within their subjective experience.
This group has bypassed much of the controversy generated by more traditional mental health practitioners. Instead, they’ve moved the focus of their research into validating a relational model of mental health based on the principles of interpersonal neurobiology.
Dan Siegel and Allen Schore, who oversee a series of textbooks on Interpersonal Biology at W. W. Norton, are at the cutting edge of this.
Therapists who want to read more about the two opposing trends happening in the field of mental health can go here: http://coprofdevcenter.org/seminars/professional-seminars-for-mental-health-practitioners/
Janae B. Weinhold, PhD LPC
Colorado Springs
Pingback: Perry: Rhythm Regulates the Brain | "Don't Try This at Home"